Article originally published Fall 2020 in The Monitor magazine.
Before COVID-19 brought the world to a halt, life stood still for the Hardwick family. For Scott Hardwick, 45, of Lancaster, it stopped completely – four times in one day.
On Jan. 28, Scott’s day presumably started much like any other. The routine details – getting out of bed, making coffee and leaving the house to tend to his family- owned grooming shop – are lost to him completely. But there is one thing he remembers: the will to survive.
As he was preparing to open the doors of Hair of the Dog’s Wee Care Pet Salon in Lancaster for another day of business, an ominous chest pain prompted Scott
to leave the porch of his shop and head across the street. Sitting caddy corner to 534 Harrison Ave. was the first in a long line of Scott’s saving graces: Lancaster Fire Department Engine House No. 2.
“It’s not even really a memory, it’s more of a feeling that I had,” Scott said. “As I was walking across the street to the fire station, I just had this unshakeable feeling of, ‘I have to make it, I have to make it.’”
He almost did. Scott collapsed against the door of the fire station.
A QUICK RESPONSE
Inside Engine House No. 2, the crew was completing morning chores and preparing for the day ahead. In the midst of the morning bustle, two of the men heard a sound that caught their attention: a thud at the door. Firefighter and paramedic Kevin Nagle peeked outside to find Scott – unresponsive and struggling to breathe – at his feet. He turned to shout his discovery to co-worker Corey Snoke, and within seconds, the fire house was teeming with activity.
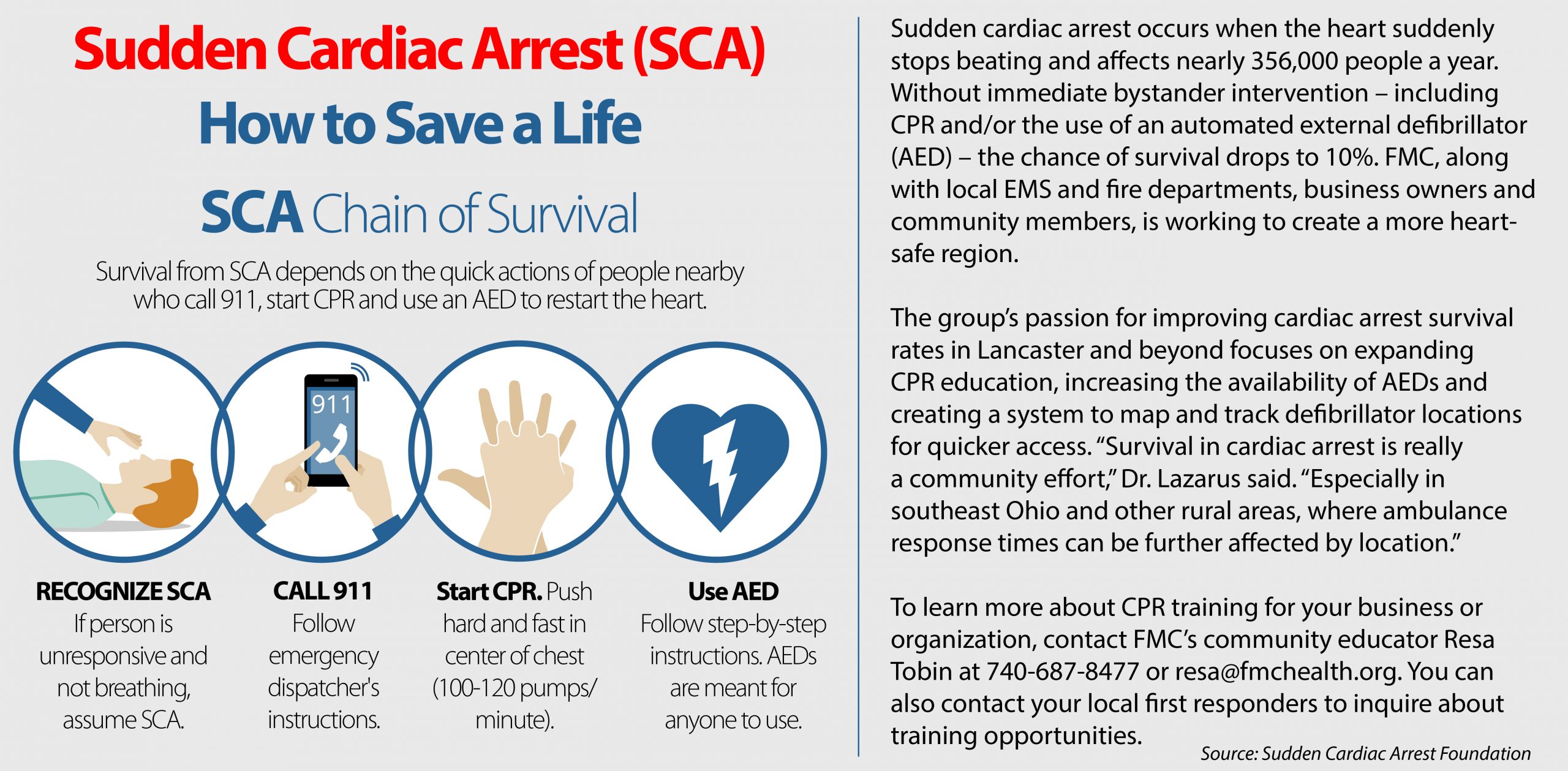
The crew soon determined that Scott was experiencing sudden cardiac arrest: something was disturbing the rhythm of his heart, causing it to flutter and quiver erratically instead of pumping blood to the rest of his body. This condition, called ventricular fibrillation (V-Fib), is particularly dangerous, but can often be corrected with an electrical shock. As some members of the department performed CPR, others connected their automated external defibrillator (AED) to Scott’s chest, delivering a successful shock to his struggling heart.
His heart beating normally once more, Scott began to tell the crew how he hadn’t felt well that morning – but within minutes, and without warning, he coded again. Another shock from the AED. Another return to consciousness. The crew repeated this intense cycle of revival a total of three times while en route to Fairfield Medical Center, keeping Scott alive even when his body was seemingly determined to give up. “Between episodes, Scott was alert and talking,” paramedic Dirk Ingram remembered. “At one point, he even looked at us and asked,‘I just died, didn’t I?’”
Scott maintained consciousness as the ambulance neared the hospital, but as they pulled into the bay of the Emergency Department at FMC’s Main Campus, he went down again. This time, his heart didn’t respond to the electrical jolt from the AED. Fortunately, the next of his saving graces was already waiting in the wings.
MIRACLE ON EWING ST.
The paramedics transferred Scott to the waiting care of FMC’s STEMI Call Team, a group of experts specially trained to respond to emergent, life- threatening heart attacks. One of those team members was interventional cardiologist John Lazarus, MD, PhD, of Fairfield Healthcare Professionals Cardiology.
As Dr. Lazarus assessed the situation, a group of six FMC team members performed CPR on Scott for nearly 30 minutes, rotating at regular intervals to avoid fatigue while continuously providing measured, high-quality chest compressions. With their hands acting as his heart, this simple yet invaluable action replaced Scott’s defunct circulatory system – an effort that would go on to play a significant role in his successful recovery.
Because Scott’s heart rhythm was no longer responding to the electrical shock of the defibrillator, Dr. Lazarus quickly consulted with cardiothoracic surgeon P. Aryeh Cohen, MD, and pulmonologist and critical care provider Jarrod Bruce, MD. Together, they made the decision to try something FMC had never attempted before: in order to give Scott any chance of survival, they would need to place him on ECMO life support immediately – in the middle of the Emergency Department.
Prior to Scott’s arrival, the team had received extensive training for the use of ECMO, a technology that artificially replaces the heart and lungs, in controlled environments – like the operating room, Cath Lab and ICU – all of which are prepped and ready with the necessary equipment. This was a different ball game, but the team didn’t bat an eye. Staff members raced through the hospital to gather the supplies they would need to save the life of the husband and father who so desperately needed their help – they collected everything from cutting-edge technology to simple extension cords, and they did it in record time.
“One of the great things about FMC is the fact that we have the opportunity to create strong, trusting relationships with our teams,” Dr. Lazarus recalled of making the uncommon decision. “Everybody jumped into action and was awaiting direction, allowing us to start ECMO within 34 minutes of Scott’s arrival to the ED – which is remarkably fast.”
With the ECMO device in place and acting as Scott’s heart and lungs, it was time for the team to identify the cause of his life- threatening heart rhythm disturbance. In the Cath Lab, Dr. Lazarus discovered a 100% blockage of Scott’s left anterior descending (LAD) artery. “Because this vessel supplies such a large portion of the cardiac muscle with oxygen, blockages can cause serious – and often fatal – complications, earning it the name the ‘widow maker,'” said Dr. Lazarus. Fortunately for Scott’s wife, Sally, the condition didn’t have a chance to live up to its name on that January day. “They saved my life that morning, too,” she later said of her husband’s survival.
With the artery stented, blood flow restored and a balloon pump in place to assist his recovering heart, the team prepared Scott for transfer to The Ohio State University Wexner Medical Center for ongoing critical care. While his vitals were stable, questions remained about Scott’s cognitive function: had his brain suffered any damage from the repeated stopping of his heart? Through CPR, the use of AEDs, and quick, decisive action, the Lancaster Fire Department and FMC’s team had done everything they could to save Scott’s life and return him to full health – but had it been enough? In a week’s time, they would find the answer was a resounding “yes.”

A LIFE OF GRATITUDE
After spending a week and a half in the ICU, Scott slowly regained consciousness and began to fill in the holes of his story with the help of his family, care providers and community. It was then that he learned just how many people had worked together to save his life. And while Scott’s journey has been physically and emotionally taxing, it has also been full of gratitude.
For Dr. Lazarus, Scott’s story serves as a reminder of his motivation as a physician. “Scott’s story really hit home for me. He’s similar in age to me with a lovely family and a job that he loves – and it all could have been lost,” Dr. Lazarus said.
“After his transfer, the one thing that reassured me was knowing that we had provided him with cutting-edge care and a good chance for survival here at FMC. And when I heard that he had made a full neurologic recovery and would be able to regain the rhythm of his daily life – that was the most heartwarming for me.”
And as Scott continues to recover, growing stronger with each cardiac rehab session and receiving encouraging news with each diagnostic test, his follow-up visits with Dr. Lazarus have been anything but ordinary. The two, linked by such an incredible story, share a unique bond.
“The last time I saw him, Dr. Lazarus walked into my appointment, shook my hand, shook his head, and said, ‘Still a miracle,’ ” Scott recalled. “He reminds me not to dwell on the past, to keep moving forward – and I want to give him my thanks every time I see him.”
Scott is reminded of his renewed appreciation for life on a daily basis. When he looks at his wife and daughter, who kept the family business open while he recovered, he is filled with pride. When he sees the fire station across the street from his shop, he is reminded of his gratitude. And when he meets members of the FMC team that helped save his life, there are no words to fully convey his thanks.
“By the grace of God, someone inside that fire station heard me that morning,” Scott said. “And FMC’s response was so choreographed, like they’d done it a thousand times before. I know it all could have ended differently that day, and that puts a lot of things into perspective.”
To learn more, about Cardiovascular Services at Fairfield Medical Center, click here.